Welcome back to the Neuroscience Meets Social and Emotional Learning Podcast, episode #120 with a review and my experience using of the Fisher Wallace Brain Stimulator from episode #108 with Kelly Roman.
*NOTE: Andrea Samadi did not receive any incentive or royalty for this review for the Fisher Wallace sleep device. Anyone can test this device, in exactly the same way, as they do offer a 30 day trial period through their website.
REVISION ADDED APRIL 5th/2021 at 9:58 marker with TIPS from Kelly Roman, Fisher Wallace Co-founder and CEO.
You will learn:
✔︎ What to expect if you want to try the Fisher Wallace Brain Stimulator to improve your sleep, anxiety or mood.
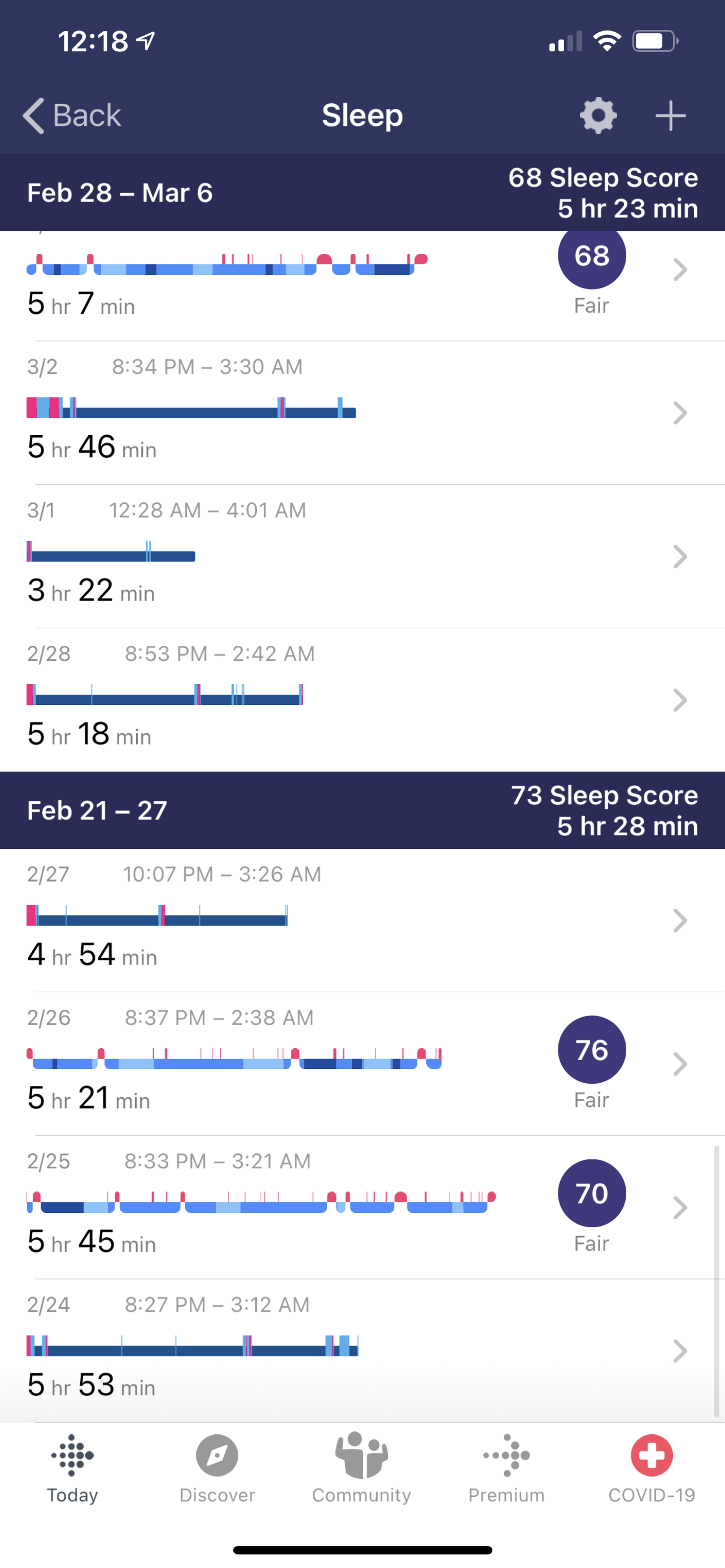
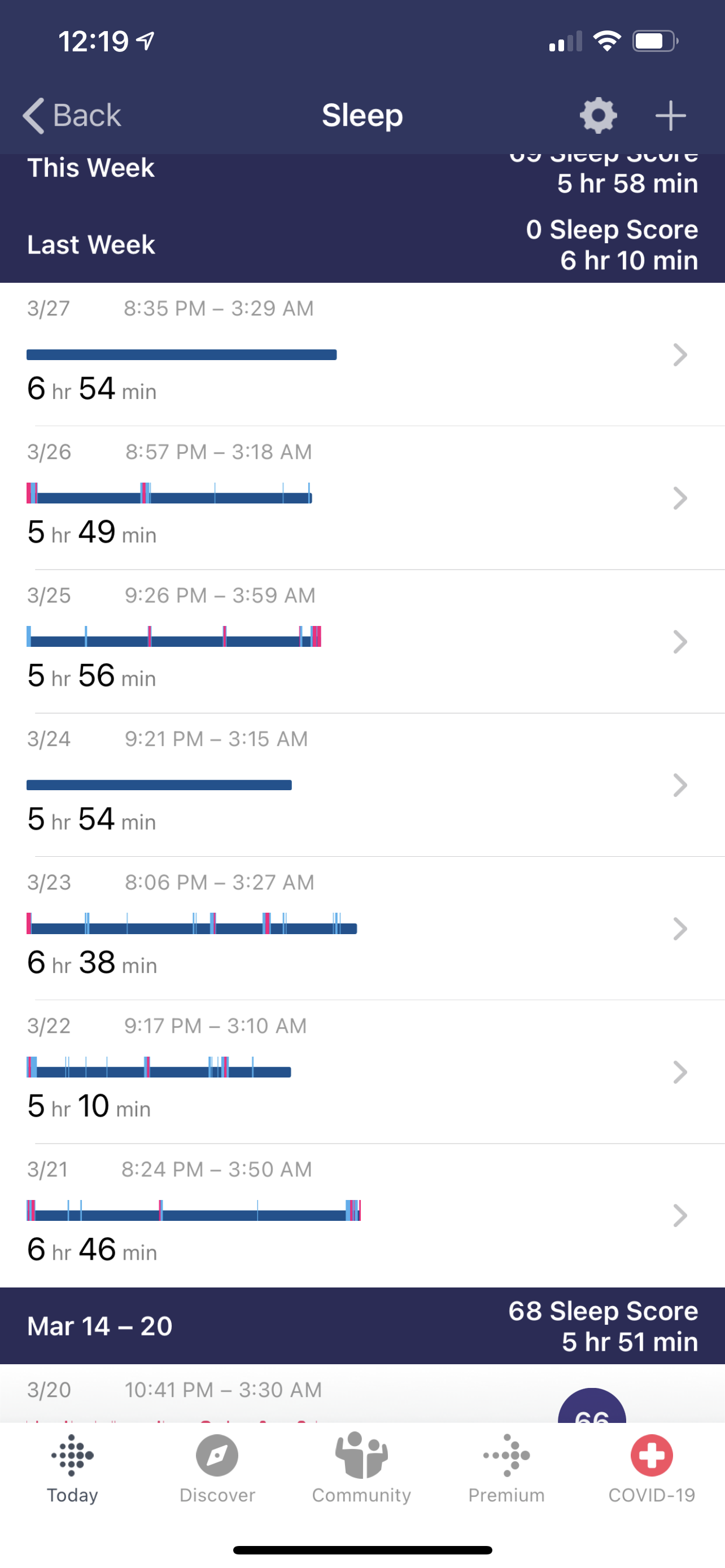
✔︎ How Andrea Samadi measured and tracked her sleep, using the FitBit App, and improved her sleep from getting around 5 hours and 28 minutes in her baseline week to hitting close to 7 hours of sleep in her final days of the trial.
✔︎ How you can try the Fisher Wallace Brain Stimulator for Improved Sleep, Reduced Anxiety or Depression.
Access past episodes here: https://lnkd.in/grfaE7y
Hello and Welcome back! I’m Andrea Samadi, a former educator who has been fascinated with learning the science behind high performance strategies in schools, sports and the workplace, for the past 20 years. If you have been listening to our podcast for some time, you will know that we’ve uncovered that if we want to improve our social and emotional skills, and experience success in our work and personal lives, it all begins with putting our brain health first. We’ve mentioned that sleep is one of the top 5 health staples that’s a known brain-health and Alzheimer’s prevention strategy, from our episode #87[i] helping us to take our results, productivity and health to these higher levels, so when I had the opportunity to improve my sleep, I jumped on the chance, with the hopes that with what I learn from my experience, could help you, or someone you know who might be struggling with getting enough sleep each night. There isn’t a day that goes by that I don’t hear someone in my network mention that they are working on improving their sleep.
If you want to hear the episode with Kelly Roman[ii], the CEO of Fisher Wallace Labs and their wearable medical devices to help improve sleep, while also treating anxiety and depression, go back and listen to episode #108. After this interview with Kelly Roman last February of 2021, I shared with him that my brain scan at Amen Clinics (in July 2020)[iii] showed what Dr. Shane Creado felt my brain showed signs of sleep deprivation, and Kelly graciously offered to send me one of the devices/paired with a Fitbit see if we could improve my sleep. I accepted the offer and promised to take the month-long trial seriously. It’s just a few days after the end of the month, and the results are in.
But first, if you’re interested in this device, contact Fisher Wallace Labs[iv] at www.fisherwallace.com or by calling 1-800-692-4380. For just under $500 (they show a discount on their website when I last checked) you will be mailed a kit with the simulator, electrode headset, Velcro headband, sponges, carry case, manual, and shipping label. The Fitbit is separate if you want to measure your results like I did, and something you can purchase on your own. They offer a 30-day Refund Policy.
There are videos that you can watch that show you how to use the device right on their website.[v] When I received the Fisher Wallace device, it came quickly, via Fedex, and was simple and easy to set up, after I watched a video through their website.
Here’s what I learned:
Before doing the month-long trial of wearing the device, Kelly suggested getting a baseline for my sleep, and measure at least 3 days without using the device, to see the quality and quantity of sleep beforehand. I wanted to get the most accurate reading of how I was sleeping before I tested the device, so I did everything I knew would help my sleep like eliminating alcohol one week prior and during the baseline so I knew it wouldn’t interfere and setting the stage for a good night sleep each night.
Just a note: I have a strange sleep schedule, going to bed by 8:30pm each night and waking by 3:30am, which is a 7-hour slot. I live in Arizona and choose this sleep time mostly because the summers are hot, and it’s helpful to be able to hit the hiking trails early morning, see the sunrise, and beat the heat that gets well above 110 degrees in the summer.
My baseline was shocking, and if you have never measured your sleep, I highly suggest doing this as a starting point. In that 7-hour slot, I was only averaging 5 hours and 28 minutes of sleep each night, and this was with me really trying during my baseline measurement.
IMAGE OF BASELINE RESULTS FROM THE FITBIT APP:
After week 1 of using the device twice a day, for 20 minutes, I felt a surge of energy as well as a clear head, but that first week I had a couple of things that I had to complete late into the night, and it threw off my schedule for that week. Also, being a Mom, there are times the kids wake up at night, and that threw it off this week.
After week 2, I was averaging 6 hours and 23 minutes of sleep each night. This was a significant jump. So for the 7 hour block, it was saying that I was sleeping for most of that block, and not awake for an hour or so, like the baseline week showed. When the baseline week showed I was up an hour or so, this wasn’t me up, walking around, doing work or anything. This was the fact that without the machine, the quality and quantity of my sleep was much less.
After week 3, I was close to 6 hours of sleep each night, and week 4 and 5 breaking the 6 hour mark again averaging 6 hours and 10 minutes.
With what I know about sleep, just from the research I have been doing, and from my brain scan conversation with Dr. Shane Creado, a sleep expert who works with elite athletes, I know that I can still improve my sleep from getting 6 hours to 7 hours, but this would mean not waking up as early and I know that for the time being this is the best slot, so I will see how close to 7 hours of sleep I can get using the device.
This whole experience has given me a lot to think about, and far more understanding with how to create more energy in the day by using a device that was designed to relax your brain and improve sleep. It clearly has improved mine.
Here are the specific weekly results:
Baseline Week 1 (Feb 21-28) Averaged 5 hours and 28 minutes of sleep).
2/24: 5 hours and 53 minutes sleep. (took 10 minutes to fall asleep, 5 times awake, 11 times restless and 48 minutes awake)
2/25: 5 hours 45 minutes sleep. 1 hour 3 minutes awake SLEEP SCORE 70
2/26: 5 hours 21 minutes sleep. 40 minutes awake. SLEEP SCORE 76
2/27: 4 hours 54 minutes of sleep. (took 15 minutes to fall asleep, 3 times awake, 5 times restless and 25 minutes awake).
2/28: 5 hours 18 minutes of sleep. 31 minutes awake.
Using Device for 20 minutes 2x/day
WEEK 1 (averaged 5 hours and 23 minutes of sleep)
3/1: 3 hours 22 minutes (first day using the device I had a deadline and had to work well past my bedtime to meet it. This happens sometimes, but I wasn’t tired after just 3 hours of sleep and felt energized on day 1 of using the machine.
3/2: 5 hours 46 minutes. 58 minutes awake.
3/3 5 hours 7 minutes. 53 minutes awake. SLEEP SCORE 68
3/4 5 hours 37 minutes. 34 minutes awake.
3/5 6 hours 34 minutes 18 minutes awake.
3/6 5 hours 58 minutes 1 hour awake. (kid up in the night).
WEEK 2 (averaged 6 hours and 3 minutes of sleep).
3/7 6 hours 46 minutes with 26 minutes awake.
3/8 6 hours 17 minutes with 38 minutes awake.
3/9 6 hours and 12 minutes. SLEEP SCORE 79
3/10 5 hours 56 minutes. SLEEP SCORE 74
3/11 6 hours 15 minutes awake 24 minutes.
3/12 5 hours 16 minutes. SLEEP SCORE 76
3/13 5 hours 36 minutes. SLEEP SCORE 66
WEEK 3 (averaged 5 hours and 51 minutes of sleep).
3/14 6 hours 3 minutes. SLEEP SCORE 71
3/15 5 hours 29 minutes. SLEEP SCORE 68
3/16 6 hours and 18 minutes with 37 minutes awake.
3/17 6 hours and 28 minutes with 28 minutes awake.
3/18 6 hours and 19 minutes with 45 minutes awake.
3/19 6 hours and 7 minutes with 41 minutes awake.
3/20 4 hours and 13 minutes with SLEEP SCORE 66.
WEEK 4 (averaged 6 hours and 10 minutes of sleep).
3/21 6 hours 46 minutes with 49 minutes awake.
3/22 5 hours and 10 minutes with 39 minutes awake.
3/23 6 hours and 38 minutes with 43 minutes awake.
3/24 5 hours and 54 minutes forgot to wear fitbit. Don’t know how many min. awake.
3/25 5 hours and 56 minutes with 56 minutes awake.
3/26 5 hours and 49 minutes with 27 minutes awake.
3/27 6 hours and 54 minutes. Forgot to wear fitbit.
WEEK 5 (averaged 6 hours and 10 minutes of sleep).
3/28 5 hours and 51 minutes with 21 minutes awake.
3/29 5 hours and 36 minutes with 23 minutes awake.
3/30 5 hours and 52 minutes with SLEEP SCORE 69.
3/31 6 hours and 51 minutes with 42 minutes awake.
IMAGE OF FINAL WEEK RESULTS FROM THE FITBIT APP:
TRIAL OVER
4/1 5 hours 22 minutes with 33 minutes awake. DIDN’T USE DEVICE.
4/2 6 hours and 53 minutes with 34 minutes awake. USED DEVICE.
Mood and Anxiety
I did notice some other improvements in addition to sleep, and I know the device also helps to improve your mood, anxiety and depression. While depression does run in my family, and it’s something I am fully aware of, it’s not something I’ve encountered any symptoms with to date, and I think this might that I’m aware of the fact that I need a certain amount of exercise to keep the endorphins and neurotransmitters flowing.
But I did notice that I had more patience, was less high strung or anxious, and was calmer with my day-to-day activities. I noticed this change immediately (and so did my husband) and along with an increase of energy, I was able to complete more tasks, in less time, and felt less stress before going to sleep.
Final Evaluation
I will continue to use the Fisher Wallace Brain Stimulator, maybe not every day, as I do want to continue to measure and see how I do without it, but I’d love to get my sleep into the 7-hour range, because I know this would help me in many other areas of my life. If you would like to try the device, and have any questions at all for me, please feel free to contact me with your questions. [vi]
In the meantime, if you want to learn more about tips to improve your sleep, I recommend going back to some of our podcasts that dive deep into the importance of sleep, like episode #71 on Self-Regulation and Sleep with a Deep Dive into Dr. Shane Creado’s “Peak Sleep Performance for Athletes”[vii] or episode #85 with Dr. Sarah McKay on “High Performing Brain Health Strategies that We Should All Know About and Implement.”[viii]
See you later next week with episode #121 with Paul Zientarski, who is the former PE teacher from Naperville, IL where I will dive deep into exactly what their program entailed to achieve the outstanding results that put them on the map for the most compelling case study proving the profound impact that exercise has on our cognitive abilities.
See you next week!
SLEEP STUDY REVISION (added April 5th/2021) at marker (9:58).
After I released my sleep study episode, I sent it over to Kelly Roman from Fisher Wallace Laboratories, and he let me know that there were some important considerations that I should mention to further improve this episode, to go a bit deeper into the sleep study results. He suggested that I read the article “How to Interpret the results of a sleep study”[1] that had some important terminology that he felt was important to mention.
The article explains Total Sleep Time
“The total sleep time is the total amount of sleep time scored during the total recording time. This includes time from sleep onset to sleep offset and is distributed throughout the sleep time as minutes of Stage N1 sleep, Stage N2 sleep, Stage N3, and rapid eye movement (REM) sleep. All these times are described in minutes. A low total sleep time may indicate that the patient slept for an insufficient period of time due to non-medical/non-physiological reasons, certain medical or sleep disorders, or as a result of the effect of medications. Long total sleep time may suggest prior sleep deprivation, medical conditions, or effects of medications. High levels of sleep fragmentation, as defined by recurrent awakenings and/or stage shifts may result in complaints of non-restorative sleep even when an apparently normal total sleep time is present.” (How to Interpret the Results of a Sleep Study).
A Fitbit does measure these sleep stages, and in my study, I showed the total time I was asleep in the 7-hour block of time, and minutes awake but didn’t share the REM time since I only got this report with a sleep score. I’m not sure why some days I didn’t get a sleep score. If I was to repeat this study, or go deeper into my results, I could look at the stages of sleep and REM time to see how much deep sleep I’m getting using the device vs without the device. Looking at the scores, I can see that in my baseline week I was averaging 42 minutes of REM sleep and 58 minutes in my last week using the device.
Sleep Efficiency
“Sleep efficiency is another important parameter that refers to percentage of total time in bed actually spent in sleep. It is calculated as sum of Stage N1, Stage N2, Stage N3, and REM sleep, divided by the total time in bed and multiplied by 100. Sleep efficiency gives an overall sense of how well the patient slept, but it does not distinguish frequent, brief episodes of wakefulness. A low sleep efficiency percentage could result from long sleep latency and long sleep offset to lights on time with otherwise normal quantity and quality of sleep in between. Many laboratories report total wake time, that is, the amount of wake time during the total recording time in minutes after the sleep onset. The total amount gives a general estimation for overall quality of sleep. Total wake time is the reciprocal of total sleep time. A high total sleep time percent is always associated with low total wake time percent and vice versa.” (How to Interpret the Results of a Sleep Study)
I looked up sleep efficiency and found a calculator[2] to help figure out this time and I’m not sure how accurate this calculator is, but this is a start for taking a closer look at the data from my sleep study.
BASELINE: To see my sleep efficiency in my baseline, I took 2/24 where I went to sleep at 8:27pm and woke up at 3:12am. I used the sleep efficiency calculator to see how efficient it says my sleep was in the baseline period. It calculated that I was in bed for 423 minutes, (7.1 hours) was awake 1.3 hours, and had a sleep efficiency score of 82%.
FINAL WEEK: I took the last day of the study, 3/31 and where I went to sleep at 7:56pm and woke up at 3:29am. The calculator logged 454 minutes of sleep (7.6 hours) with 57 minutes awake, and a sleep efficiency score of 87%.
Wakefulness After Sleep Onset (WASO)
Another important reported parameter is “wake after sleep onset, also known as ‘WASO’. This refers to periods of wakefulness occurring after defined sleep onset. This parameter measures wakefulness, excluding the wakefulness occurring before sleep onset. WASO time is a better reflection of sleep fragmentation.” (How to Interpret the Results of a Sleep Study).
The Fitbit measures total time awake, and I did log this time in my results. This was the part of the study that I found to be a bit shocking, since I just assumed that when I went to sleep around 8:30pm, that I was sleeping until I woke up around 3:30am or so. I didn’t know that during my 7-hour block of time, I was averaging 53 minutes of wakefulness in my baseline and only 29 minutes of wakefulness in my last week of testing. It’s definitely eye-opening to see how the device improved my sleep WASO score.
In my baseline, I was showing an average of 47.2 minutes awake or WASO and in the final week of the study, WASO score was significantly improved, averaging 36.8 minutes using the device.
Kelly Roman suggested that I look at each week using the device, compared to the baseline of 5 hours and 28 minutes of sleep, (323 minutes) showing week 1 not much change due to that one night I worked late with 323 total minutes of sleep , week 2 showed an increase in 35 minutes of sleep, Week 3 an increase of 23 minutes, week 4, an increase of 42 minutes, and week 5, the same increase of 42 minutes above the baseline. According to Kelly Roman, 20 minutes of sleep increase is what he says would be the gold standard minimum that doesn’t seem like a lot but allows for improved REM sleep and over time he says reduces sleep debt. What was powerful was that my study showed an increase of much more that this gold standard of 20 minutes improvement showing me that the device worked better than I realized without showing him these results.
He also suggested the importance of talking about drug therapy for sleep improvement, where a drug like Ambien would be clinically significant to improve total sleep time by 20 minutes per night, and my results showed to be much higher than this. The Fisher Wallace Device is an incredible tool for improving sleep without using any medicines, but it’s important to note-- I’ve heard over and over again from Dr. Daniel Amen of the negative impacts that sleep aids have on the brain saying “They cause memory problems, daytime drowsiness, confusion, addiction and severe withdrawal syndrome if they are abruptly discontinued”[3] If you are listening to this episode, using a doctor prescribed sleep medicine, please do speak to your doctor before making any changes to your health care plans.
I hope this additional information on my sleep study was helpful for you, if you know that sleep is something that you want to improve. I am going to continue to improve mine, and so grateful to have had this opportunity to test the Fisher Wallace Sleep Device.
UPDATE ONE YEAR AFTER THIS REVIEW: Don't miss Andrea's RECAP of this episode a year later, answering the question "One year later, do you still use the Fisher Wallace device?"
RESOURCES:
The Secret to Overcoming Sleep Problems by Dr. Daniel Amen June 25th, 2019 https://www.amenclinics.com/blog/the-secrets-to-overcoming-sleep-problems/
[1] How to Interpret the results of a sleep study by Deepack Shrivastava, MD Published Nov. 25, 2014 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4246141/
[2] https://mysleepwell.ca/cbti/sleep-efficiency-calculator/
[3] Sleeping Pills, Anxiety Meds, and the Impending Disaster by Dr. Daniel Amen, June 11, 2020 https://www.amenclinics.com/blog/sleeping-pills-anxiety-meds-and-the-impending-disaster/
REFERENCES:
[i] Neuroscience Meets Social and Emotional Learning Podcast EPISODE #87 with Andrea Samadi on “The Top 5 Brain Health and Alzheimer’s Prevention Strategies” https://www.achieveit360.com/the-top-5-brain-health-and-alzheimers-prevention-strategies-with-andrea-samadi/
[ii] Neuroscience Meets Social and Emotional Learning Podcast EPISODE #108 with Kelly Roman, the CEO of Fisher Wallace Laboratories on “Wearable Medical Devices for Anxiety, Depression and Sleep/Stress Management” https://andreasamadi.podbean.com/e/ceo-of-fisher-wallace-laboratories-on-wearable-medical-devices-for-anxiety-depression-and-sleepstress-management/
[iii] Neuroscience Meets Social and Emotional Learning Podcast EPISODE #84 BRAIN SCAN RESULTS “How a Spect Scan Can Change Your Life” with Andrea Samadi PART 3 https://andreasamadi.podbean.com/e/how-a-spect-scan-can-change-your-life-part-3-with-andrea-samadi/
[iv] https://www.fisherwallace.com/ 1-800-692-4380
[v] https://www.fisherwallace.com/
[vii] Neuroscience Meets Social and Emotional Learning Episode #71 on a Deep Dive into Dr. Shane Creado’s “Peak Sleep Performance for Athletes” https://www.achieveit360.com/self-regulation-and-sleep-with-a-deep-dive-into-dr-shane-creados-peak-sleep-performance-for-athletes/
[viii] Neuroscience Meets Social and Emotional Learning Episode #85 with Dr. Sarah McKay on “High Performing Brain Health Strategies that We Should All Know About and Implement.” https://www.achieveit360.com/neuroscientist-dr-sarah-mckay-on-high-performing-brain-health-strategies-that-we-should-all-know-about-and-implement/
No comments yet. Be the first to say something!